What are pathogenic bacteria?
Any bacteria that is capable of causing disease in an organism is considered pathogenic bacteria.
Some species of bacteria may be pathogenic in one species but not in another. Pathogenic bacteria are often expressed differently depending on genetic and health-related factors. For example, some people may harbour a pathogenic bacterium but never develop the associated disease, likely due to genetic factors.
Immunocompromised individuals are far more likely to develop symptomatic disease than healthy individuals. The symptoms and presentation of bacterial disease also often vary between species and even between individuals. All this being said, the vast majority of bacteria are either beneficial or entirely harmless.
Characteristics of pathogenic bacteria
Pathogenic bacteria have a set of characteristics that allow them to adapt to their specific host, and also make them potentially dangerous for them too. Here's a list of the characteristics of pathogenic bacteria:
The most important characteristic of pathogenic bacteria is that they can cause disease in an individual or a species.
Pathogenic bacteria (like any bacteria) can multiply rapidly. They can reproduce quickly, especially in the right conditions, like the moist and warm human body. The important point of pathogenic bacteria in terms of reproduction is that they do it by using the host's resources.
Pathogenic bacteria are communicable: they are transmitted from one infected individual to another by a variety of methods (detailed later on in the article).
They can develop resistance to antibiotics: Some pathogenic bacteria have developed resistance to antibiotics, making them more difficult to treat and control.
Some pathogenic bacteria can produce toxins that can cause serious illness or death.
Pathogenic bacteria interact with the immune system of the host, with two possible outcomes: avoid the immune system, or be attacked by it.
Difference between other pathogens and pathogenic bacteria
- Viruses: Unlike bacteria, viruses are not alive, so they are not affected by antibiotics. Viruses are capable of causing disease in all living organisms, including bacteria. COVID-19 is a timely example of a virus.
- Fungi: These are eukaryotic organisms (like us!) that consist of mushrooms, molds, and more. Only a small number of fungi are pathogenic. An example of a pathogenic fungus would be Candida albicans, which can cause candidiasis, also known as a yeast infection.
- Parasites: Any organism that lives within or on a host species and depends on them for survival is a parasite. Parasites can vary greatly in size and taxonomy. Parasites include tapeworms, ticks, and helminths.
- Bacteria: Bacteria are a diverse group of prokaryotic (single-celled) organisms found everywhere on Earth. The vast majority of bacteria are harmless and many are quite beneficial, while a small number are pathogenic and can cause serious diseases in humans and non-human animals. Bacteria can usually be treated effectively with antibiotics, though antibiotic resistance is a
growing problem .
Cause of pathogenic bacteria infection
Pathogenic bacteria infections occur when harmful bacteria are consumed or come into contact with the body. If the immune system doesn't act fast enough, the bacteria can reproduce inside the host's cells or in the interstitial tissue, causing damage through their increase in numbers or by the synthesis and release of toxins.
Infection by pathogenic bacteria can happen through a variety of means, including:
Consuming contaminated food: Pathogenic bacteria can be found in a variety of food products, including meats, poultry, seafood, dairy products, and fruits and vegetables. Consuming food that has been contaminated with these bacteria can cause illness. Therefore, it's important to clean and cook food properly, to reduce the chances of eating contaminated food.
Coming into contact with infected animals or animal faeces: Pathogenic bacteria can be found in the faeces of infected animals and coming into contact with these bacteria can cause illness.
Poor hygiene: Not washing hands or surfaces properly can lead to the spread of pathogenic bacteria.
Exposure to contaminated water: Pathogenic bacteria can be found in contaminated water sources, such as lakes and rivers, and coming into contact with these bacteria can cause illness.
Exposure to infected individuals: Some pathogenic bacteria can be spread through contact with infected individuals, such as through sneezing or coughing.
It is important to take proper precautions, such as practising good hygiene, properly storing and preparing food, and avoiding contact with contaminated water sources, to prevent pathogenic bacteria infection.
Examples of pathogenic bacteria
Bacteria can cause a variety of symptoms and diseases. Some examples of pathogenic bacteria include Clostridioides difficile, E. coli, Staphylococcus aureus, and Helicobacter pylori. In the following paragraphs, we will discuss these examples of pathogenic bacteria in more detail.
Gram-positive pathogenic bacteria
Gram-positive pathogenic bacteria species will provide a positive (violet-coloured) result on a Gram stain test (Fig. 1) and have a thick peptidoglycan layer forming the cell wall. The thick cell wall absorbs antibiotics, thus rendering Gram-positive bacteria more susceptible to antibiotics that target the cell wall than Gram-negative bacteria.
 Figure 1: Gram-positive bacteria from a Gram stain test. Source: Wiki
Figure 1: Gram-positive bacteria from a Gram stain test. Source: Wiki
Gram-positive pathogenic bacteria, example 1: Clostridioides difficile
Clostridioides difficile, commonly referred to as C. diff, is a potentially pathogenic Gram-positive bacteria species capable of causing severe diarrheal illness in humans and some non-human animal species. Pathogenic strains of C. difficile (e.g., strains that create entero- or cytotoxins) cause severe inflammation of the colon (colitis), with symptoms that include profuse, bloody diarrhea and severe abdominal pain. In a small minority of cases, this colitis can become so severe that colectomy (surgical removal of the colon) is required and can result in death.
C. difficile has developed antibiotic resistance and can be very difficult to eradicate. The most common antibiotics used to treat C. difficile are metronidazole and vancomycin, though the relapse rate is high (roughly 20%) even after successful treatment. While the most commonly mentioned risk factor for C. difficile infection is antibiotic use, other risk factors, such as gastroenteritis and laxative abuse, may be of equal importance. Nearly 500,000 people are estimated to experience symptomatic C. difficile infection annually, resulting in nearly 30,000 deaths.
Gram-positive pathogenic bacteria, example 2: Staphylococcus aureus
Staphylococcus aureus is a Gram-positive bacteria that is usually a harmless commensal (symbiotic) bacteria that can become pathogenic. When pathogenic, S. aureus can cause abscesses, food poisoning, bacteremia, and more. Some strains of S. aureus have developed antibiotic resistance. An example of one such resistant strain is methicillin-resistant S. aureus (MRSA). Some strains of S. aureus can be successfully treated with penicillin. In 2017, nearly 120,000 Americans suffered from S. aureus-related bacteremia, resulting in around 20,000 deaths.
Methicillin-resistant S. aureus (MRSA) is a particularly common infection among the elderly and immunocompromised in hospitals and nursing homes, but it is also commonly encountered in gyms, prisons, childcare facilities, and among intravenous drug users. MRSA is most commonly treated with vancomycin.
Gram-negative pathogenic bacteria
Gram-negative pathogenic bacteria species will provide a negative result on a Gram stain test, as they are not able to retain the violet colour and will instead be shown as pink or red (Fig. 2). Unlike Gram-positive bacteria, Gram-negative bacteria have a thin peptidoglycan layer forming their cell wall and are less susceptible to antibiotics that target the cell wall. Gram-negative bacteria are particularly dangerous, as they are more difficult to eradicate and are prone to developing resistance to antibiotics.

Gram-negative pathogenic bacteria, example 1: Escherichia coli
Escherichia coli is a Gram-negative bacteria usually found in the intestines of humans and most other mammals, as well as birds. Most strains of E. coli are harmless commensals of the microbiome, but a few strains can cause disease in humans. The most common symptoms of E. coli infections are typical of other gastrointestinal illnesses- abdominal cramping and diarrhoea. However, infection by some strains, particularly those that produce Shiga toxins, can result in colitis and even perforation of the bowel.
E. coli is most often spread through the consumption of contaminated food or liquid, particularly poorly cooked ground meats and raw fruits and vegetables. E. coli is considered to be the principal cause of traveller’s diarrhoea worldwide. As E. coli infections are often self-limiting, the main treatment consists of fluid replacement to prevent dehydration. In some cases, antibiotics such as ciprofloxacin or rifaximin are used and can be effective. It is estimated that around 265,000 people experience symptomatic E. coli infection annually, resulting in only around 100 deaths.
Shiga toxins, named after Japanese scientist Kiyoshi Shiga, are toxins produced by some forms of Gram-negative bacteria, specifically certain strains of E. coli and Shigella dysenteriae, the causative bacteria species in dysentery.
Gram-negative pathogenic bacteria example 2: Helicobacter pylori
Helicobacter pylori is a Gram-negative bacteria that is the most common cause of peptic ulcer disease in humans. Most H. pylori infections are asymptomatic (it is estimated that around 50% of the human population is infected) but, when disease does occur, ulcers can form in the stomach and the duodenum (the first portion of the small intestine). Symptoms commonly include heartburn, melena (black, tarry faeces containing blood due to upper gastrointestinal bleeding), nausea, and upper abdominal pain. In some cases, H. pylori peptic ulcer disease can eventually result in gastric cancer. Treatment of H. pylori primarily consists of two antibiotics (e.g., clarithromycin and amoxicillin) and a proton pump inhibitor (PPI). Like many other species of pathogenic bacteria, H. pylori is developing resistance to antibiotics.
Until 1982, peptic ulcer disease was believed to have been caused by diet (e.g., acidic foods) and stress. The proposition that the disease may in fact be caused by a species of bacteria was initially met with hostility from the broader medical community. In order to prove these sceptics wrong, an Australian physician named Barry Marshall drank a broth containing H. pylori, developed symptomatic peptic ulcer disease, and then cured his disease with antibiotics. In 2005 he, along with his collaborator Robin Warren, were awarded the Nobel Price for their efforts.
Mycobacteria as pathogenic bacteria
Mycobacteria consist of nearly 200 bacteria species of the genus Mycobacterium. Due to the high levels of mycolic acid they produce, mycobacteria cannot be visualized through the usual Gram stain procedures, and are therefore neither Gram-positive or Gram-negative. Instead, mycobacteria are known as acid-fast bacteria, which require acid-fasting staining techniques in order to be visualized. Many species of mycobacteria are known to cause severe disease in mammals, including humans.
Mycobacteria pathogenic bacteria example 1: Mycobacterium tuberculosis
Mycobacterium tuberculosis is the causative agent of tuberculosis in humans and non-human primates. While the vast majority (around 90%) of individuals infected with M. tuberculosis will have latent disease (asymptomatic), it can result in severe disease in symptomatic individuals. Treatment consists of a combination of at least four antibiotics (ethambutol, isoniazid, pyrazinamide, and rifampicin) for several months. Antibiotic resistance is becoming a major problem and even today it is estimated that around 1.5 million people die due to M. tuberculosis annually, mostly within the developing world.
Most people with symptomatic disease will develop the classic pulmonary symptoms (e.g., chest pain and coughing up blood), but some will develop what is known as extrapulmonary tuberculosis. Extrapulmonary tuberculosis can be challenging to diagnose, as the symptoms and complications can be virtually indistinguishable from other diseases. This has led to M. tuberculosis being referred to as “the great mimicker”.
Mycobacteria pathogenic bacteria example 2: Mycobacterium leprae
M. leprae is a slow-growing mycobacteria species (Fig. 3) that causes leprosy in humans and some non-human mammals. Due to its slow growth, M. leprae can take years or even decades to cause symptomatic leprosy. The disease typically results in nerve damage that leads to skin damage and, eventually, disfigurement. In severe cases, blindness, paralysis, and severe disfigurement may occur. M. leprae can be successfully treated using a combination of three antibiotics (clofazimine, dapsone, and rifampicin) for several months and antibiotic resistance is relatively rare. It is estimated that over 200,000 people develop leprosy annually, more than 50% of which are in India.
 Figure 3: M. leprae (the small red rods). Source: Wiki Commons
Figure 3: M. leprae (the small red rods). Source: Wiki Commons
Pathogenic bacteria in blood
One of the most deadly forms of bacterial infection occurs when pathogenic bacteria make their way into the bloodstream. This can happen either with an immediate entry of the bacteria into the bloodstream, for example through an infected intravenous needle, or following increased severity of a primary infection in a different part of the body. This primary infection could include things like an infected tooth, a wound on the forearm, an intestinal infection - the list goes on - where the bacteria present in this primary infection eventually travel to the bloodstream.
When pathogenic bacteria infect the blood, it is called bacteremia. Bacteremia is very dangerous, as it can quickly result in sepsis, septic shock, and, often, death. It can also cause the infection to spread through the circulatory system to other portions of the body, for example to the brain or cardiac tissue. Bacteremia can be caused by both Gram-positive and Gram-negative species of bacteria.
Pathogenic bacteria in food
Pathogenic bacteria can also be present in food. Bacteria can multiply rapidly at certain temperatures, known as the "danger zone," between 5°C and 60°C, the temperatures at which food is usually at. Food left in this temperature range for too long can become contaminated with harmful bacteria, which is why it's called the "danger zone".
To prevent the growth of pathogenic bacteria in food, it is important to properly store, handle, and prepare food. This includes keeping cold food at or below 4°C and hot food at or above 60°C and avoiding cross-contamination between raw and cooked food. Proper sanitation and hygiene, such as washing hands and surfaces frequently, also help to prevent the spread of bacteria.
Preservation methods such as refrigeration, freezing, and canning can also help to prevent the growth of bacteria in food. Refrigeration slows the growth of bacteria, while freezing stops it entirely. Bacteria, however, are not necessarily killed by freezing. Canning, through the process of heating the food to a high temperature for a certain time, kills any bacteria present and creates a vacuum seal that prevents contamination.
It is also important to cook food to a safe internal temperature to kill any bacteria present. This includes cooking meat, poultry, and eggs to a minimum temperature, as well as reheating leftovers to 74°C to kill bacteria.
Overall, pathogenic bacteria in food are a serious concern and it is important to take proper precautions to prevent contamination and ensure the safety of the food we consume.
Pathogenic Bacteria - Key takeaways
- Any bacteria that is capable of causing disease in an organism is considered pathogenic bacteria.
- When pathogenic bacteria infects the blood, it is called bacteremia.
- Pathogenic bacteria are characterised by causing harm to their host, reproducing using the host's resources, interacting with the host's immune system and being communicable. Some pathogenic bacteria can also develop antibiotic resistance or produce toxins.
- Pathogenic bacteria can be transmitted from one host to another by various methods, including direct host-to-host transmission, but also contaminated food or water.
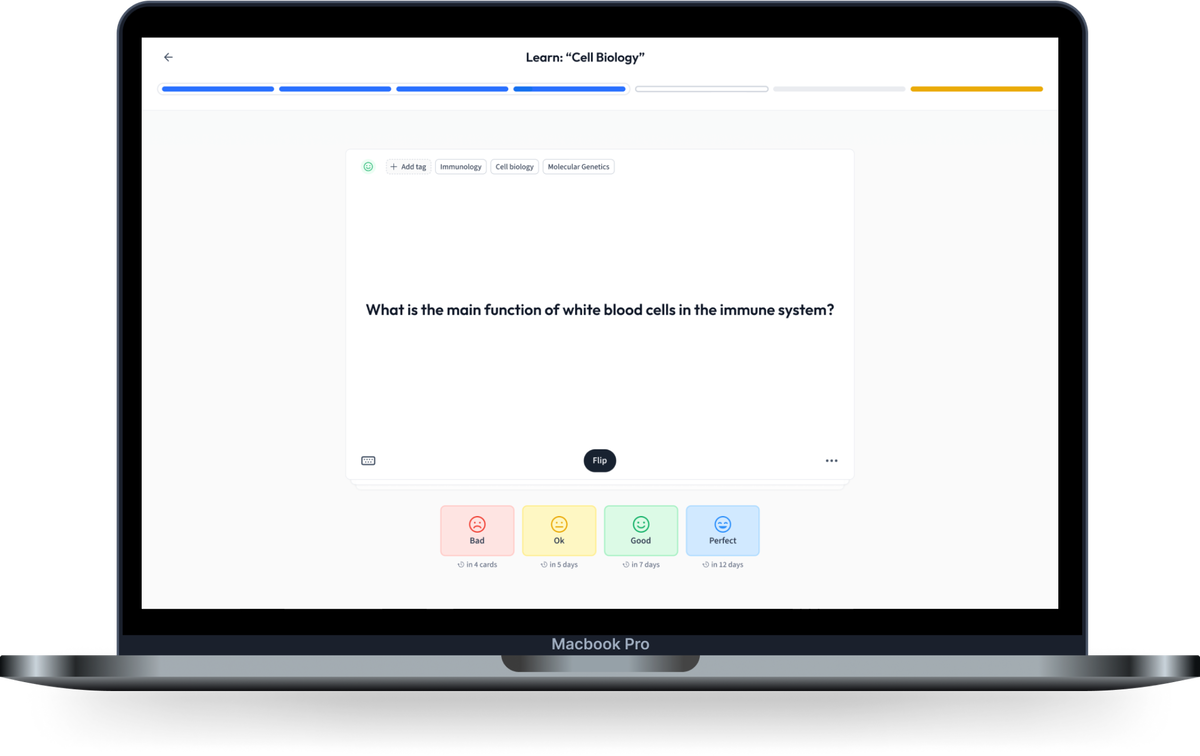
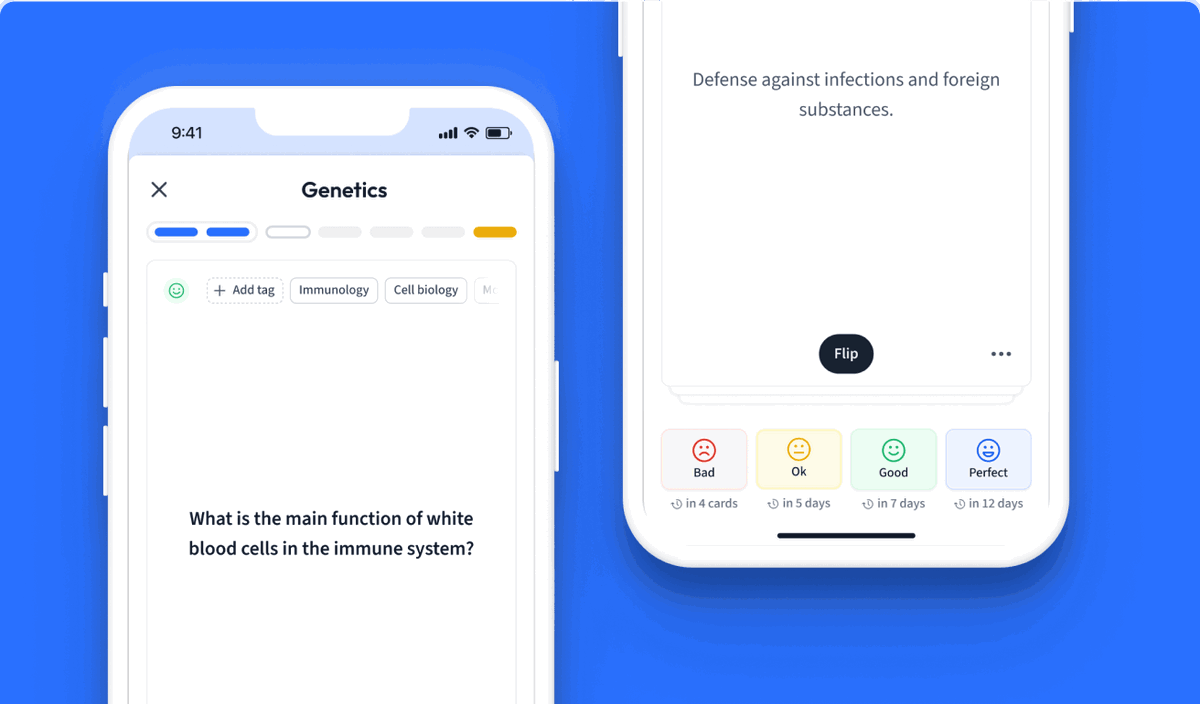
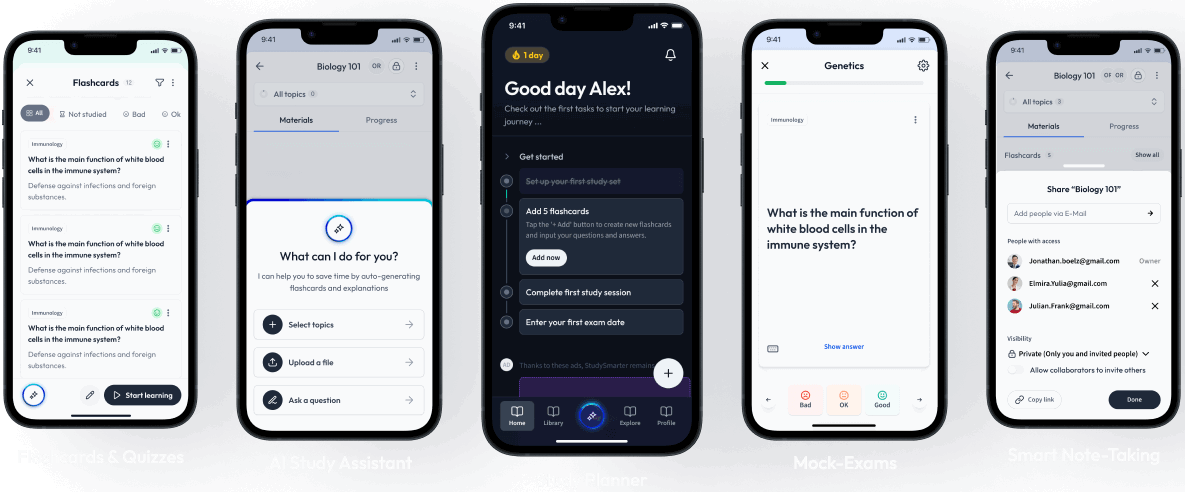
Learn with 18 Pathogenic Bacteria flashcards in the free StudySmarter app
We have 14,000 flashcards about Dynamic Landscapes.
Already have an account? Log in
Frequently Asked Questions about Pathogenic Bacteria
How to destroy pathogenic bacteria?
There are many ways to destroy pathogenic bacteria. The most known way is with antibiotics once an infection or disease has started. However, measures can be taken prior to the infection to destroy bacteria: sterilizing food with heat, preserving food with salt and other spices, or wiping surfaces with disinfectants are just a few examples of how to destroy pathogenic bacteria.
Are all bacteria pathogenic?
No, not all bacteria are pathogenic. Some are even beneficial or essential for the correct functioning of the human body, like the bacteria present in the gut or vagina microbiota.
What are pathogenic bacteria?
Pathogenic bacteria are any bacteria that are capable of causing disease in an organism.
What per cent of bacteria are pathogenic?
Only 5% of bacterial species are pathogenic. Pathogenic microorganisms (including bacteria) constitute only 1% of all known microorganisms up to date.
Is nail fungus a pathogenic bacteria?
No, nail fungus can be caused by several fungi, but not bacteria. However, bacteria can cause nail infections. The bacteria that usually cause nail infections are Pseudomonas aeruginosa and Klebsiella spp.
Where can pathogenic bacteria grow and reproduce?
Pathogenic bacteria grow on the organisms they infect, but they can also survive on other inorganic or organic matter, like water or faeces.
Depending on the strain of bacteria, the colonised organism or body part will differ. For example, some bacteria grow on human lungs, while others grow on plant leaves.
Additionally, some bacteria might grow and reproduce inside the hosts' cells, but most bacteria actually multiply in the tissue fluid of the invaded organ, not inside cells.
What do pathogenic bacteria cause?
Pathogenic bacteria cause infections and disease. Some examples of these diseases are tetanus, typhoid fever, bacterial pneumonia, syphilis, etc.
How do pathogenic bacteria cause disease?
Pathogenic bacteria usually cause disease through damage to the infected tissue through replication or the production of toxins.
However, bacterial infections can also induce damage to the host by activating the immune response to such an extent that it attacks not only the bacteria or the pathogen-infected cells, but also the host's own healthy cells.
How many pathogenic bacteria are there?
Only 5% of bacterial species are pathogenic. Pathogenic microorganisms (including bacteria) constitute only 1% of all known microorganisms up to date.


About StudySmarter
StudySmarter is a globally recognized educational technology company, offering a holistic learning platform designed for students of all ages and educational levels. Our platform provides learning support for a wide range of subjects, including STEM, Social Sciences, and Languages and also helps students to successfully master various tests and exams worldwide, such as GCSE, A Level, SAT, ACT, Abitur, and more. We offer an extensive library of learning materials, including interactive flashcards, comprehensive textbook solutions, and detailed explanations. The cutting-edge technology and tools we provide help students create their own learning materials. StudySmarter’s content is not only expert-verified but also regularly updated to ensure accuracy and relevance.
Learn more