Understanding Antibiotic Resistant Bacteria: The Basics
Antibiotics have been one of the most amazing discoveries for mankind, effectively battling multiple sorts of bacterial infections. However, just like in every battle, enemies learn to adapt. In this case, our enemy is the Antibiotic Resistant Bacteria. Outsmarting, mutating, surviving - this is how these resilient strains of bacteria become magnificently resilient to the very drugs designed to eliminate them.
Before you delve any further, let's get familiar with the keyword of this learning - Antibiotic Resistant Bacteria.
Definition of Antibiotic Resistant Bacteria
The medical world defines Antibiotic- Resistant Bacteria as microorganisms that have evolved and adapted to become immune or resistant to the antibiotics that were initially effective in treating them. They pose a serious global threat to public health due to their ability to make pharmaceutical treatments ineffective, leading to higher medical costs, prolonged hospital stays, and increased mortality.
Take the case of Methicillin-resistant Staphylococcus aureus (MRSA), for example. This notorious one has gained a reputation for causing difficult-to-treat infections in hospitals worldwide. Once susceptible to the antibiotic methicillin, it has now evolved to become resistant, giving healthcare professionals a tough time in dealing with it.
Mechanisms of Antibiotic Resistance in Bacteria
Isn’t it intriguing how bacteria can cunningly fend off our medical artillery? This section will shed light on how bacteria adapt to survive despite the strong selection pressure of antibiotics.
There are four primary mechanisms for antibiotic resistance in bacteria:
- Drug Inactivation or Modification
- Alteration in Target Molecule
- Decreased Drug Uptake
- Increased Drug Efflux
Let's take a closer look. Drug inactivation or modification, as the name suggests, involves bacterial enzymes that deactivate the antibiotic. This can happen through enzymatic degradation or modification of the antibiotic. The alteration in the target molecule is when the antibiotic can no longer bind to the bacterial cell due to mutations, making the drug ineffective. Decreased drug uptake occurs when the bacterial cell alters its membrane permeability, limiting the antibiotic's access into the bacteria. Lastly, Increased drug efflux is when the bacteria actively pumps the antibiotic out of the cell using efflux pumps.
Understanding these mechanisms is crucial, for it helps us see the bigger picture of how antibiotic resistant bacteria have become such a significant issue in public health.
Causes behind the Emergence of Antibiotic Resistant Bacteria
Few would dispute the impact of antibiotics in shaping modern medicine, but with these benefits comes a sobering reality. The rise of antibiotic resistant bacteria has taken centre stage in global health discussions. Unveiling how the simple act of treating an illness could create superbugs seems paradoxical, but in fact, it's quite rational when examined closely.
Major Causes of Antibiotic Resistance
The development of antibiotic resistance is a complex issue. It is influenced by multiple factors, acting independently or synergistically.
When you say 'antibiotic resistance', it refers to the ability of bacteria to withstand the effects of an antibiotic that they ordinarily would be susceptible to.
Firstly, overuse and misuse of antibiotics is a significant contributor. When antibiotics are overused, it gives bacteria more opportunities to adapt and develop resistance.
Incorrect diagnosis leading to unnecessary prescriptions, use of antibiotics in livestock for growth promotion, and patients not completing a prescribed antibiotic course are all factors contributing to this overuse and misuse.
A classic example of antibiotic misuse is using antibiotics to treat viral infections such as the common cold or flu. Since antibiotics are designed to fight bacteria, not viruses, this use not only proves ineffective but also contributes to the problem of antibiotic resistance.
Secondly, poor infection control in healthcare settings can contribute to the spread of antibiotic-resistant bacteria.
Next, the natural genome evolution of bacteria also plays a critical role. Given the rapid multiplication rate of bacteria, mutations that confer resistance to antibiotics can quickly spread in bacterial populations.
Evolution of Antibiotic Resistance in Bacteria
Understanding the evolutionary aspect of antibiotic resistance is key to comprehend how bacteria become invincible against the power of antibiotics.
The evolutionary process of bacteria works according to the principles of natural selection. In an environment with antibiotic pressure, bacteria susceptible to the antibiotic die, while those with mutations that confer resistance survive. These resistant bacteria then reproduce, passing along their resistant genes to the next generation.
In genetics, the process of passing genes from an organism to its offspring is known as heredity. It plays a prominent role in the evolution of antibiotic-resistant bacteria, as the resistance genes are passed on to successive bacterial generations.
Evolution can occur through various mechanisms like mutation and horizontal gene transfer.
A mutation, a change in an organism's genetic material, may result in resistance to an antibiotic. On the other hand, horizontal gene transfer is when an organism transfers genetic information to another organism that is not its offspring. This usually occurs via the exchange of plasmids – small, circular pieces of DNA. If a plasmid carrying resistance genes is shared, antibiotic resistance can spread rapidly within a bacterial population.
Both processes are natural and inevitable, but human actions, such as misuse of antibiotics, can accelerate them. It's always better armed with knowledge as you navigate the world of biology, and we hope that this comprehensive look into the mechanisms and causes behind the emergence of antibiotic-resistant bacteria has been enlightening.
Known Examples of Antibiotic Resistant Bacteria in Ecosystems
Your journey into the world of antibiotic-resistant bacteria wouldn't be complete without understanding the real-life examples of these persistent microorganisms. Let's dive into the details and explore some of the prominent antibiotic-resistant bacteria that are impacting our ecosystems today.
Listing Known Antibiotic Resistant Bacteria
It's important to remember that antibiotic resistance is not an isolated incident, and it is not limited to a single type of bacteria. Many different types of bacteria have developed resistance to antibiotics, and they each pose unique challenges to health professionals worldwide.
This section lists some of the most well-known antibiotic-resistant bacteria:
- Methicillin-Resistant Staphylococcus aureus (MRSA): As previously mentioned, MRSA is one of the most notorious antibiotic-resistant bacteria due to its ability to cause severe skin infections and other health issues.
- Klebsiella pneumoniae: It has gained significant attention due to its resistance to carbapenems, a group of antibiotics often considered as the last line of treatment for severe bacterial infections.
- Pseudomonas aeruginosa: Known for its intrinsic resistance mechanisms, this bacteria is notorious for causing hospital-acquired infections, particularly in patients with weakened immune systems.
- E. coli: While some strains are benign, others like the Extended-Spectrum Beta-Lactamases (ESBL) producing E. coli, have developed resistance to multiple antibiotics, posing a significant health risk.
Hospital-acquired infections (HAIs) serve as perfect examples of how antibiotic resistant bacteria can wreak havoc. Patients admitted to the hospitals for unrelated ailments often end up dealing with new infections caused by antibiotic-resistant bacteria. The prevalence of HAIs by organisms such as MRSA and K. pneumoniae only underscores how crucial it is to manage the problem of antibiotic resistance.
Effects of Antibiotic Resistant Bacteria on Ecosystems
Antibiotic-resistant bacteria not only pose a threat to human health but also have far-reaching impacts on ecosystems. These resilient bacteria can spread across ecosystems, impacting various biotic and abiotic factors.
Here are a few major impacts of antibiotic-resistant bacteria on ecosystems:
Firstly, antibiotic-resistant bacteria can be transmitted to animals, impacting their health and contributing to the overall burden of antibiotic resistance.
Zoonotic diseases are diseases that can be transmitted between animals and humans. The transmission of antibiotic-resistant bacteria can often take place through this route.
Secondly, the presence of antibiotic-resistant bacteria in environments such as water bodies can impose a threat to the ecosystem's biodiversity. Exposed organisms can either die due to the inability to compete with these enhanced bacteria or evolve themselves, indirectly influencing the food chain and affecting biodiversity equilibrium.
Lastly, antibiotic-resistant bacteria in the environment can also contribute to the genetic pollution. The phenomenon of horizontal gene transfer that we had earlier discussed allows these resistance genes to be transferred to other non-resistant bacterial strains, thus, further propagating the problem.
Another aspect worth noting is the role of human activities in spreading antibiotic resistance across different ecosystems. Factors such as sewage and waste water discharge, agricultural runoff containing animal faecal matter, and even medical waste can lead to the proliferation and distribution of antibiotic-resistant bacteria in the environment. It indeed paints a picture of how interconnected the pieces of the antibiotic resistance puzzle are.
As you venture further into the exploration of antibiotic-resistant bacteria, shed light on their mechanisms, causes and the challenges they pose, not just to humans, but to whole ecosystems as a whole.
Strategies for Preventing Antibiotic Resistant Bacteria
The fight against antibiotic resistant bacteria might sound formidable, but it's far from a lost cause. Armed with knowledge and informed strategies, you can play a significant role in combating this challenging problem. Let's delve into the key strategies that could help prevent the spread of antibiotic resistant bacteria.
Steps in Preventing the Spread of Antibiotic Resistant Bacteria in Ecosystems
Halting the spread of antibiotic resistant bacteria in ecosystems requires a concerted and multifaceted approach. This approach comprises of measures that span everything from policy level interventions to individual actions. The steps involved can be systematically categorized into a few broad areas:
Policy interventions are decisions made by governments or organisations to regulate activities, often aimed at achieving beneficial outcomes or minimising harmful effects. In the context of antibiotic resistance, policy interventions can include regulation of antibiotic use, funding for research, or implementation of infection control measures.
Here are several important steps in this regard:
- Responsible Use of Antibiotics: The prudent use of antibiotics in medicine and agriculture is paramount. This includes prescribing and using antibiotics only when necessary, and always completing the full course of the medication even if the symptoms have improved.
- Vaccination: Vaccines reduce the need for antibiotic use by preventing bacterial infections in the first place. The more people that are protected by vaccinations, the fewer will need antibiotics and the less likely bacteria are to develop resistance.
- Regulatory Measures: Governments must regulate the use of antibiotics, especially in agricultural practices. Restricting the use of medically important antibiotics for growth promotion in farm animals can play a vital role in controlling antibiotic resistance.
- Infection Control Practices: Implementing stringent infection control practices in healthcare settings can prevent the spread of antibiotic resistant bacteria.
- Research and Development: Continued research into new antibiotics and alternative treatments is needed as bacteria continue to develop resistance to existing antibiotics.
Interestingly, the areas mentioned above are interconnected. For instance, the responsible use of antibiotics can lead to a reduced need for new antibiotics, thereby creating less pressure for the development and approval of new drugs. Similarly, expanding vaccination coverage can reduce the overall need for antibiotics, thus reducing the potential for misuse. This systemic view illustrates the complexity of preventing antibiotic resistance.
The Role of Education in Preventing Antibiotic Resistant Bacteria
Education plays a pivotal role in the fight against antibiotic resistant bacteria. Informing individuals, healthcare workers, and policymakers about the dangers of antibiotic resistance and the importance of responsible antibiotic use can lead to significant improvements in the current state of antibiotic resistance.
This educational approach can help ensure that antibiotics are used responsibly by all stakeholders. Here are some key aspects of this education:
Stakeholders, in this context, include anyone who can affect or is affected by antibiotic resistance. This includes individuals, health professionals, policymakers, agricultural workers, researchers, and even bacteria themselves!
- Understanding Antibiotics: It’s important to educate individuals about what antibiotics are, how they work, and when their use is appropriate. As highlighted before, antibiotics are ineffective against viral infections, and this crucial knowledge can help prevent their misuse.
- Recognizing Risks: Awareness of the potential dangers and consequences of antibiotic resistance can lead people to make informed decisions about antibiotic use.
- Encouraging Responsible Behaviour: Education can foster responsible behaviour, such as completing prescribed antibiotic courses, not sharing antibiotics with others, and not pressuring doctors for unnecessary antibiotic prescriptions.
- Professional Training: Nurses, doctors, and other healthcare workers should be adequately trained on the implications of antibiotic resistance and the importance of prudent antibiotic use, infection control, and patient education.
- Policy Advocacy: Educating policymakers about the significance of antibiotic resistance can help in formulating appropriate policies and regulations to tackle it effectively.
Consider a simple scenario of a patient presenting with symptoms of common cold. An educated patient would understand that antibiotics are ineffective in treating viral infections like common cold. On the other hand, an adequately trained physician would discourage inappropriate use of antibiotics, explaining the reasons to the patient. The ultimate result? Responsible use of antibiotics, reduction in risk of developing resistance, and a small but significant victory over antibiotic resistant bacteria.
Hence, implementing effective educational strategies is as critical as the adoption of direct intervention measures in preventing the rise and spread of antibiotic resistant bacteria. It's clear that a holistic approach, combining the power of education and sound prevention strategies, holds the key to winning this global fight against antibiotic resistance.
Antibiotic Resistant Bacteria: Future Predictions and Implications
Having delved deep into the world of antibiotic resistant bacteria, their mechanisms, causes, and various strategies to prevent their spread, it's crucial to shift focus towards the future. What does the continued evolution of antibiotic resistance imply for our ecosystems? Let's unfold the predictions and possible implications.
Future Prospects: The Continuing Evolution of Antibiotic Resistance in Bacteria
As fascinating as it is to study the world of bacteria and their ability to develop antibiotic resistance, it’s also sobering to realise that unless concrete action is taken, the situation is likely to worsen.
Future prospects, in this context, refer to the projected progression and potential scenarios related to the evolution of antibiotic resistance in bacteria.
Several informed predictions have been made regarding the future of antibiotic resistant bacteria:
- Increased prevalence of antibiotic resistance: Without decisive action, the prevalence of antibiotic resistant bacteria is expected to increase. This uptick would make treatment of common bacterial infections challenging, leading to higher mortality and morbidity rates.
- Broad resistance to antibiotics: Bacteria might develop resistance to multiple antibiotics, leading to a rise of 'pan-resistant' bacteria against which we have no effective drug defenses.
- Return to the pre-antibiotic era: If the issue of antibiotic resistance continues to escalate without a solution, there could be a return to the ‘pre-antibiotic era’ where even simple infections could prove fatal.
- Increased burden on healthcare: The escalation of antibiotic resistance would exert immense pressure on healthcare systems worldwide, with longer hospital stays, higher medical costs, and increased mortality rates.
A futurist scenario worth discussing is the rise of pan-resistant bacteria. Imagine a strain of bacteria resistant to every antibiotic in our arsenal. Treatment would be exceedingly difficult, with doctors left with no effective drugs to administer. This scenario, though dire, could become a reality if antibiotic resistance continues to proliferate unchecked.
Understanding the Implications of the Rise of Antibiotic Resistant Bacteria in Ecosystems
With future projections giving us a grim picture, it's only logical for you to wonder about the implications this rise of antibiotic resistant bacteria could have on our ecosystems. Will it only be limited to human health, or are there broader ecological implications to consider?
Well, the rise of antibiotic resistant bacteria holds implications far beyond human health. Here are the broader ecological concerns:
Ecological implications refer to the potential impact or consequences of an event, activity, or change on an ecosystem or environment. In this case, it is the consequences of the rise of antibiotic resistant bacteria on our ecosystems.
- Damage to ecosystems: Antibiotic-resistant bacteria could disrupt ecosystems, potentially causing harm to various flora and fauna.
- Impact on wildlife health: Wildlife could be seriously affected by exposure to antibiotic-resistant bacteria, leading to increased illness and mortality in various species.
- Pollution and habitat destruction: The spread of antibiotic-resistant bacteria could lead to widespread environmental pollution and potential habitat destruction. This could range from localised issues, such as polluted water bodies, to more global concerns, like the degradation of coral reefs due to diseased marine organisms.
- Disruption in ecological functions: The presence of antibiotic-resistant bacteria can disrupt key ecological functions. For example, bacteria play crucial roles in nutrient cycling. If antibiotic-resistant bacteria replace these beneficial bacteria, the balance of these nutrient cycles could be disturbed, impacting plant growth and ultimately, the entire food chain.
Consider the effect of antibiotic resistance on earthworms. Earthworms are decomposers that play a pivotal role in soil fertility. Antibiotics entering the soil through agricultural runoff can create a selection pressure leading to the emergence of antibiotic-resistant bacteria. These bacteria can potentially harm earthworms, disrupt decomposition and nutrient cycling, impacting soil fertility, plant growth, and ultimately upsetting ecosystem balance.
Given these factors, it's crucial to consider not only the human health impacts but also the wider ecological implications when debating the rise of antibiotic-resistant bacteria. This comprehensive understanding will help us to strategise and tackle the issue more effectively.
Antibiotic Resistant Bacteria - Key takeaways
- Antibiotic Resistant Bacteria Definition: Bacteria that have developed the ability to survive and replicate in the presence of antibiotics, often due to misuse or overuse of antibiotics.
- Mechanisms of Antibiotic Resistance in Bacteria: Primarily occurs through the principles of natural selection where surviving bacteria have mutations that confer resistance, reproduce, passing along their resistant genes to the next generation. Other mechanisms include mutation and horizontal gene transfer.
- Evolution of Antibiotic Resistance in Bacteria: Resistance emerges naturally through genetic mutations or by acquiring resistance from another bacterium.
- Preventing Antibiotic Resistant Bacteria: Steps in preventing the spread of antibiotic-resistant bacteria in ecosystems include responsible use of antibiotics, vaccination, regulatory measures, infection control practices, and research and development.
- Examples of Antibiotic Resistant Bacteria: Examples include Methicillin-Resistant Staphylococcus aureus (MRSA), Klebsiella pneumoniae, Pseudomonas aeruginosa, and E. coli.
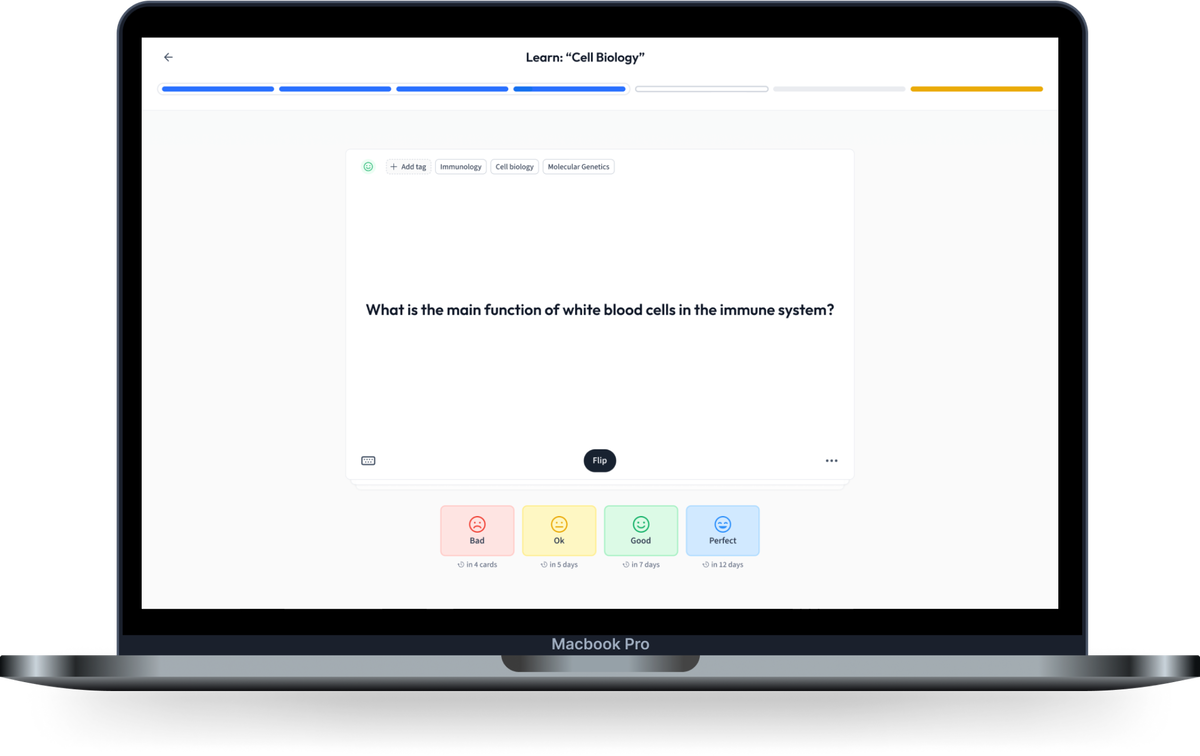
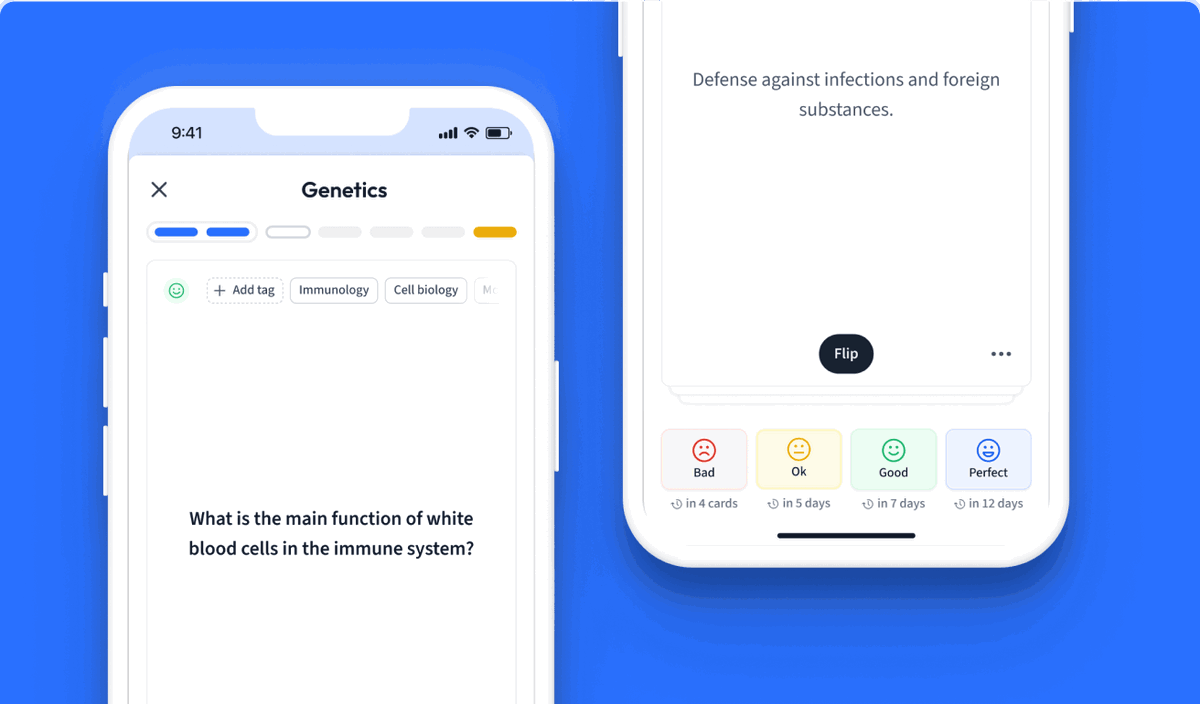
Learn with 30 Antibiotic Resistant Bacteria flashcards in the free StudySmarter app
We have 14,000 flashcards about Dynamic Landscapes.
Already have an account? Log in
Frequently Asked Questions about Antibiotic Resistant Bacteria


About StudySmarter
StudySmarter is a globally recognized educational technology company, offering a holistic learning platform designed for students of all ages and educational levels. Our platform provides learning support for a wide range of subjects, including STEM, Social Sciences, and Languages and also helps students to successfully master various tests and exams worldwide, such as GCSE, A Level, SAT, ACT, Abitur, and more. We offer an extensive library of learning materials, including interactive flashcards, comprehensive textbook solutions, and detailed explanations. The cutting-edge technology and tools we provide help students create their own learning materials. StudySmarter’s content is not only expert-verified but also regularly updated to ensure accuracy and relevance.
Learn more