Understanding Virulence in Microbiology
Virulence refers to the level of harm caused by microbes or pathogens such as bacteria, viruses, and fungi when they invade a host organism.
Breaking Down the Meaning of Virulence
Exemplifying how pathogens exert their harmful effects, virulence embodies various characteristics and factors of microorganisms, in their quest to multiply and spread. Unravelling the meaning of virulence can offer a deeper insight into the science of microbiology.Fundamentally, virulence can be quantified in terms of morbidity (sickness) or mortality (death) rates that a particular pathogen can cause within a susceptible population.
- Ability to enter the host
- Capacity to evade the host's immune response
- Potential to damage the host's tissues
| Pathogen factors | These include features of the pathogen itself, such as its genetic makeup, structure, and growth rate. |
| Host factors | They comprise the health, age, immune status, genetic makeup of the host organism. |
How Virulence Relates to Communicable Diseases
This deep connection between virulence and communicable diseases arises from the fact that many communicable diseases are caused by microbial pathogens displaying varying levels of virulence.For instance, microbial pathogens like Neisseria meningitidis show high virulence by creating severe diseases like meningitis. On the other hand, the common cold virus, Rhinovirus, exhibits lower virulence, usually only resulting in mild symptoms.
An example of this is the Measles, Mumps, and Rubella (MMR) vaccine. By administering the MMR vaccine, the virulence of these diseases is significantly reduced, consequently preventing severe illness or death.
Diving Into Virulence Factors
When studying virulence, it is essential to examine the contributing components known as virulence factors. These are molecules produced by pathogens (bacteria, viruses, fungi and protozoa) that add to their effectualness in causing disease.Discovering Key Virulence Determinants in Microbes
To fully comprehend how diseases are instigated at the microbial level, it's crucial to discover key virulence determinants. Several categories of virulence factors exist, each with a specific function or role that plays a part in how the pathogen interacts with the host. Adhesion factors, for example, allow pathogens to stick and bind to host cells, getting the process underway. Bacterial examples include pilli or fimbriae which they use to attach themselves to host tissues. Invasive factors, like bacterial enzymes, then aid in the dissemination of the pathogen through host tissues. They help in overcoming the physical barriers such as the skin or mucous membranes. Next are the two types of toxins:- Endotoxins: These are part of the bacterial cell wall in Gram-negative bacteria. Once these bacteria die or multiply, endotoxins are released, triggering an immune response.
- Exotoxins: These are proteins released by both Gram-positive and Gram-negative bacteria during their growth. Their main role is to damage or kill host cells directly.
Role of Virulence Factors in Disease Severity
The overall disease severity is directly proportional to the potency and combination of these virulence factors. Generally, more virulent pathogens produce more serious diseases, assuming all else is equivalent. Let's examine a few key roles. Starting with Adhesion Factors, these anchormen decide the initial host-pathogen contact. This contributes to disease severity since effective anchorage can lead to successful colonization, which can then increase the chances of disease manifestation. Secondly, Invasive Factors promote tissue invasion and enable the pathogen to penetrate, spread, and establish infection within the host, causing more extensive damage which translates to increased disease severity. Thirdly, the type and amount of Toxins produced can greatly affect the severity of the disease. Toxins directly damage host cells, and many have highly specific effects on particular bodily functions. Some can even manipulate the host's own immune response. Take the example of 'Superantigens', a form of exotoxins, they can cause an excessive immune response, leading to systemic inflammation and severe disease. To gauge the impact of these factors, let's consider the disease severity \( D \) is represented by the strength of the adhesion factor \( A \), multiplied by the power of the invasive factor \( I \), and the quantity of toxin \( T \), can be represented as: \[ D = A \cdot I \cdot T \] In conclusion, understanding the relationship between virulence factors and disease severity provides an invaluable perspective for biomedical research, and significantly contributes to the development of therapeutic strategies to control microbial infections.The Intricacies of Virulence Mechanisms
Microorganisms often use sophisticated virulence mechanisms to invade, colonize and cause harm to their host. These mechanisms represent the strategic tactics deployed by different pathogens, characterized by diverse operational strategies and unique molecular instruments.Decoding Virulence Mechanisms in Pathogenic Bacteria
Bacterial pathogens operate an array of virulence mechanisms. They have devised diverse pathways to triumph over host defence settings and establish infections. Entry into the host is the first exciting phase, where different bacteria deploy different invasion strategies. While some bacteria like Streptococcus pneumoniae capitalize on opportunities presented by defects in host barriers (caused by prior viral infection or injury), others like Salmonella enterica serovar Typhimurium actively invade host cells. Once inside, bacteria employ several mechanisms to elude the host's immune system. Some hide within the host cells, using them as protective shields against the host's defence. For example, Listeria monocytogenes can survive and reproduce within host's cells, thereby evading detection by the immune system. Another common strategy is the alteration of surface antigens. By continuously changing their surface proteins, some bacteria like Neisseria meningitidis can trick the immune system, which struggles to recognise and eliminate these bacteria. Certain bacteria produce substances called proteases that break down proteins, including antibodies, which impairs the host's immune response. Staphylococcus aureus, for instance, deploys proteases to resist the host's defences. Finally, bacteria employ numerous approaches to inflict harm on their host. While some release toxins that damage the host tissues, others cause harm by eliciting an excessive immune response. To illustrate the mechanism of bacterial invasion, let's use a mathematical representation. If \( B \) is the invasion by bacteria, \( E \), \( D \), and \( H \) represent entry, defence evasion, and harm mechanisms respectively, then the invasion can be represented as: \[ B = E \cdot D \cdot H \]Influence of Virulence Mechanisms on Disease Dysfunction
Various virulence mechanisms employed by bacteria directly influence disease dysfunction, typically by disrupting the normal functioning of host tissues and triggering disruptive immune responses. The degree of tissue damage often depends on the type of toxins released by the bacteria. For example, Clostridium perfringens produces alpha toxin that causes cell death, which causes extensive tissue damage and dysfunction. Severe immune response due to bacterial toxins can cause the host's immune system to damage its own cells, leading to immune-mediated tissue damage. Bacillus anthracis secretes anthrax toxins that impair immune cell function, resulting in immune-mediated damage and dysfunction of various organs. Intracellular parasitism, a phenomenon where certain bacteria hide inside host cells, leads to both cell-autonomous dysfunction (since the bacteria use the host cell's resources for their reproduction) and population-level tissue dysfunction (as the immune system unleashes a wide-scale destructive response to eliminate intracellular bacteria). Bacterial proteases not only impair the immune response but degrade extracellular matrix proteins, disrupting the structural and functional integrity of host tissues. Analysing the relationship between bacterium’s virulence mechanisms and disease dysfunction can be represented using this mathematical formula: If \( D \) is the disease dysfunction, \( T \), \( I \), \( P \) and \( M \) represent toxin-related, immune-mediated, protease-caused, and cell-autonomous mechanisms respectively, we can represent our formula as: \[ D = T + I + P + M \] Each mechanism contributes independently to disease dysfunction, highlighting the complex nature of bacterial pathogenesis.Deciphering the Difference Between Pathogenicity and Virulence
In the realm of microbiology, two crucial terms you will frequently encounter are 'pathogenicity' and 'virulence'. These terms play a fundamental role in understanding how diseases emerge and progress.Understanding Pathogenicity and Virulence: A Comparative Study
Pathogenicity and virulence, while related, refer to separate attributes of infectious pathogens. To unravel their differences, first let's understand what each term signifies. Pathogenicity refers to the capability of a microorganism to cause disease. It's a qualitative measure, which means it's about 'if' an organism can cause disease, not 'how severe' that disease might be. Virulence, on the other hand, is a measure of the severity of disease a pathogen can cause. It's a quantitative measure. Hence, it deals with 'how harmful' the disease will be when produced by a particular pathogen. Therefore, while pathogenicity classifies microorganisms into pathogenic (can cause disease) or non-pathogenic (cannot cause disease), virulence determines the extent of harm a pathogen can cause within the host. To illustrate this, consider the mathematical equation where \( P \) is the pathogenicity, and \( V \) is the virulence: \[ P = V >= 1 \] In other words, a pathogen will be categorised as pathogenic if it has any degree of virulence. Let's further examine the difference in a tabular format:| Term | Definition | Measure |
| Pathogenicity | Capability of a microorganism to cause disease | Qualitative |
| Virulence | Measure of severity of the disease a microorganism can cause | Quantitative |
Impact of Pathogenicity and Virulence on Disease Spreading
Understanding the nuances between pathogenicity and virulence helps us assess the impact of different pathogens and strategise their control. Pathogenicity essentially helps us predict whether a microorganism could evolve into a disease-causing agent. Hence, acknowledging an organism's pathogenic potential aids disease surveillance and early warning systems, allowing healthcare professionals to take preemptive measures before the actual outbreak of disease. Virulence directly influences the rate of disease spreading and its burden on populations. The higher the virulence, the more severe the disease symptoms. This can lead to increased hospitalisations, possibly more cases of long-term disability or death. Moreover, highly virulent pathogens can speed up the disease spread if they impair the host's normal functions or make the host more contagious. Taking into account several factors like pathogenicity \( P \), virulence \( V \), contagiousness \( C \) and host susceptibility \( S \), the spread of disease \( D \) across a population may be represented as: \[ D = P \times V \times C \times S \] Increased understanding of such fundamental concepts can guide more effective public health interventions and bolster our struggle against infectious diseases.Practical Applications of Virulence Studies
The practical applications of virulence studies are numerous and impactful, as they offer indispensable insights that can be utilised for effective disease control. A comprehensive understanding of virulence mechanisms allows scientists and healthcare professionals to develop efficient strategies for infection prevention and more effective treatment approaches.The Importance of Understanding Virulence in Disease Control
To devise effective disease control strategies, you must first unravel the intricate relationship between you—the host—and infectious bacteria—the pathogen. In this context, understanding the concept of virulence is of paramount importance. Virulence pertains to the capacity of a pathogen to cause damage to its host. The degree of damage inflicted can influence the disease's severity, progression, transmission, and ultimately, the outcome of disease control efforts.- Understanding Pathogenesis: Delving into the virulence factors and how they function can help interpret the intricate process of pathogenesis. This includes understanding how pathogens invade the host, avoid its immune defences, and cause harm.
- Antimicrobial Drug Design: Knowledge of specific virulence factors guided the design of antimicrobial drugs. For instance, drugs can be developed to interfere with toxin production or block mechanisms that pathogens deploy to invade host cells.
- Vaccine Development: Virulence proteins often stimulate the immune system, making them potential vaccine targets. To develop effective vaccines, understanding the contribution of various virulence factors to disease outcomes is indispensable.
- Epidemic Management: Identifying highly virulent strains can aid effective management of disease outbreaks. It involves implementing appropriate containment measures and prioritizing the allocation of healthcare resources.
How Knowledge of Virulence Contributes to Infection Prevention
Infection prevention centres around blocking the multipronged strategies that pathogens use to cause disease. Due to the diversity of pathogenic strategies, tailoring effective preventative measures requires a deep understanding of virulence mechanisms. A profoundly recurrent theme is to thwart the invasion strategies of pathogens. One method could be to develop substances that neutralize toxins used by bacteria to damage host cells and facilitate the invasion. Another approach could be to design antimicrobial drugs to inhibit the mechanisms bacteria use to attach to host cells and initiate the invasion. The ability to hide inside host cells helps multiple pathogens to escape detection and elimination by the host's immune system. In-depth knowledge of such intracellular survival strategies could be fundamental in designing therapeutic strategies to reveal these hiding pathogens to the immune system. Appreciating the role of antigenic variation—the mechanism of constantly changing surface proteins—can also guide infection prevention efforts. Vaccination strategies could be tailored to target the conserved regions of these proteins, as such regions do not change during the variation process and can be recognized by the immune system. Even the communication mechanisms among pathogens—quorum sensing—that govern collective behaviours like biofilm formation and toxin production, have been targeted to prevent infection. These are based on understanding virulence itself. In sum, the knowledge of virulence mechanisms greatly fuels the prevention of bacterial infections. We can construe the relationship as a mathematical formula, where \( V \) is the knowledge of virulence, and \( IP \) stands for infection prevention strategies: \[ IP \propto V \] Thus, improving understanding of virulence mechanisms can contribute significantly to bettering prevention strategies, providing promise for more effective control of infectious diseases in the future.Virulence - Key takeaways
- Virulence: the measure of the severity of a disease a pathogen can cause. Virulence factors play a significant role in causing disease and defending against host immune responses.
- Virulence Factors: the contributing components of virulence produced by pathogens that enhance their effectiveness in causing disease. These include adhesion factors, invasive factors, endotoxins, and exotoxins.
- Virulence Determinants: the specific categories of virulence factors that play a part in how the pathogen interacts with the host. These help in understanding how diseases are instigated at the microbial level.
- Virulence Mechanisms: the strategic tactics deployed by different pathogens to invade, colonize and cause harm to their host. These contribute to disease dysfunction and help in understanding bacterial pathogenesis.
- Difference Between Pathogenicity and Virulence: Pathogenicity refers to the capability of a microorganism to cause disease and is qualitative. Virulence, on the other hand, is a measure of the severity of the disease a pathogen can cause and is quantitative.
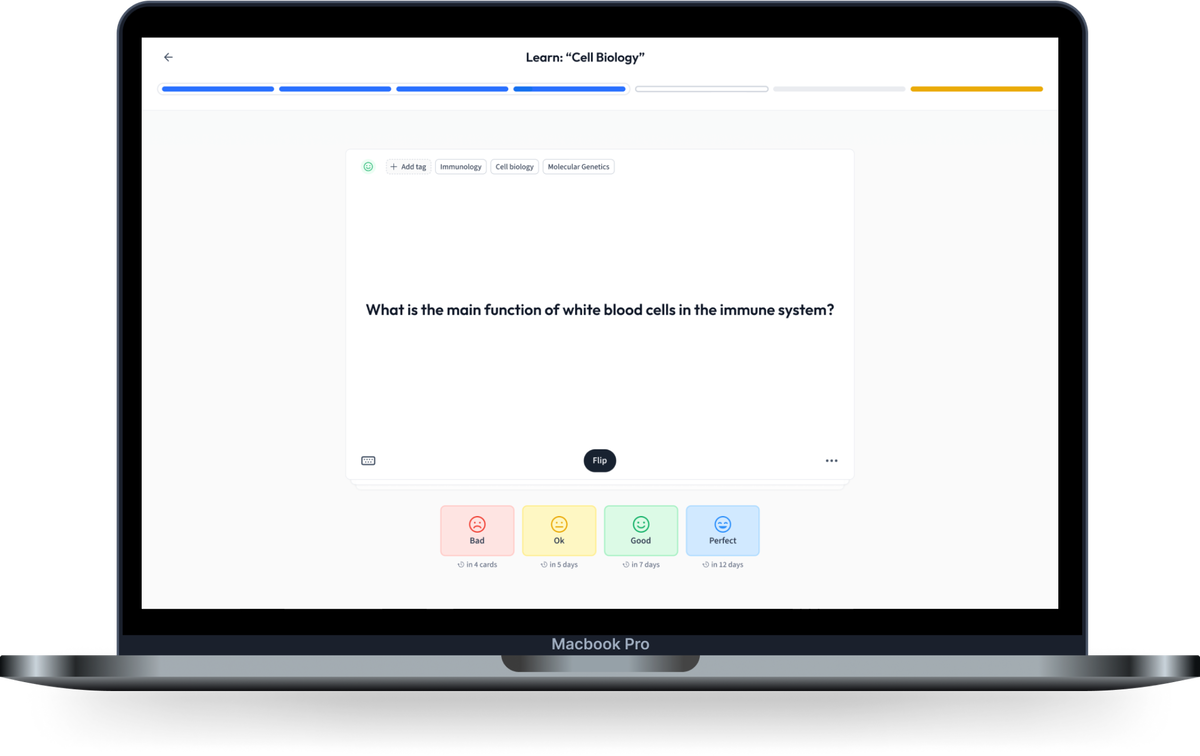
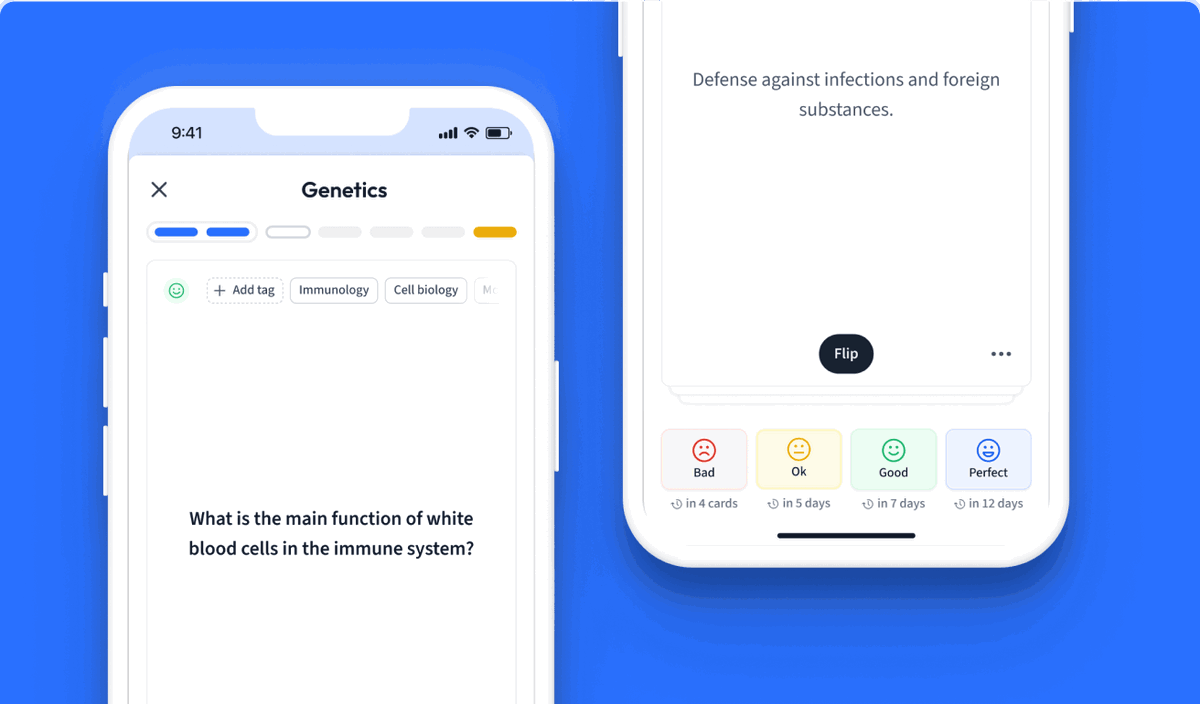
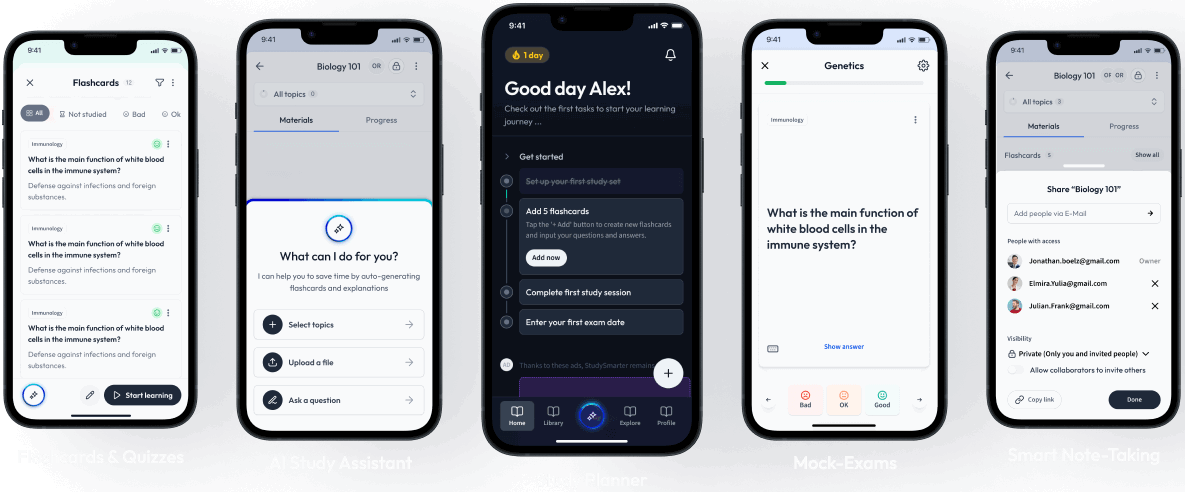
Learn with 15 Virulence flashcards in the free StudySmarter app
We have 14,000 flashcards about Dynamic Landscapes.
Already have an account? Log in
Frequently Asked Questions about Virulence


About StudySmarter
StudySmarter is a globally recognized educational technology company, offering a holistic learning platform designed for students of all ages and educational levels. Our platform provides learning support for a wide range of subjects, including STEM, Social Sciences, and Languages and also helps students to successfully master various tests and exams worldwide, such as GCSE, A Level, SAT, ACT, Abitur, and more. We offer an extensive library of learning materials, including interactive flashcards, comprehensive textbook solutions, and detailed explanations. The cutting-edge technology and tools we provide help students create their own learning materials. StudySmarter’s content is not only expert-verified but also regularly updated to ensure accuracy and relevance.
Learn more